Are you feeling uneasy about your digestive health? You’re not alone!
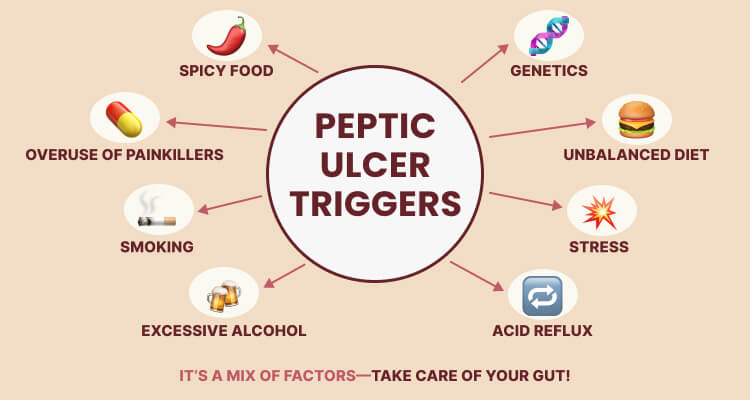
Peptic ulcers are a common concern that affects many individuals, yet they are surrounded by a web of myths and misconceptions that can obscure understanding and effective management. From the belief that spicy foods are the sole cause to misconceptions about the best dietary practices, these myths can lead to confusion and misguided choices.
Let’s delve into these prevalent myths, uncover the truths, and empower ourselves with the right knowledge for a healthier digestive journey.
Myth 1: Eating spicy food is the sole reason for peptic ulcers.
Many people see spicy foods as the enemy of the stomach. While it’s true that spicy dishes can irritate an already sensitive stomach, they are not the direct cause of ulcers. The real culprits behind ulcer formation are Helicobacter pylori (H. pylori) infections and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen.
Research indicates that H. pylori is present in approximately 70-90% of individuals who experience peptic ulcers. Therefore, you should get tested for H. pylori. Also, consider including kitchen spices like cumin and oregano. However, it is not recommended to eat spicy food if you have heartburn, as it can further irritate the stomach lining.
Myth 2: Dairy milk is a long-term solution to heal peptic ulcers.
A common belief is that sipping a glass of dairy milk will soothe peptic ulcer discomfort. While it may provide temporary relief by coating your stomach, it can trigger stomach acid production, resulting in greater discomfort later on.
The misconception comes from the initial soothing effect, but milk can worsen symptoms. Instead, for acid peptic reflux, you can try these herbal teas to soothe symptoms:
- Chamomile Tea – Reduces inflammation and soothes the stomach lining.
- Licorice Root Tea (Deglycyrrhizinated Licorice – DGL) – Helps coat and protect the esophagus and stomach.
- Fennel Tea – Helps digestion and reduces bloating without increasing acid production.
What to Avoid
-
- Peppermint Tea – Can relax the esophageal sphincter and worsen reflux.
- Ginger Tea (in excess) – While helpful for digestion, too much can increase acid production.
Myth 3: I’m too young to worry about acid peptic ulcers.
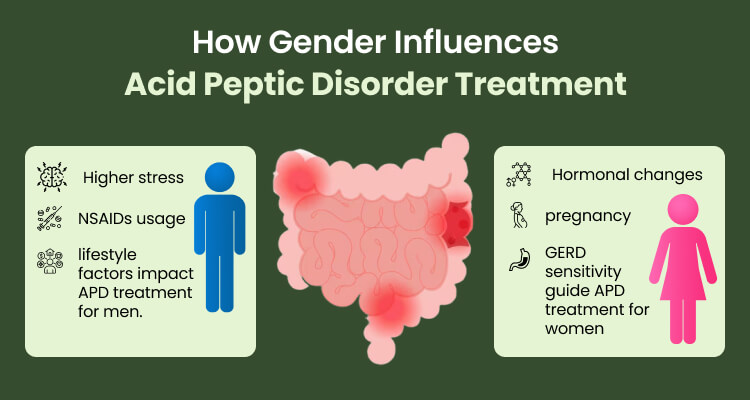
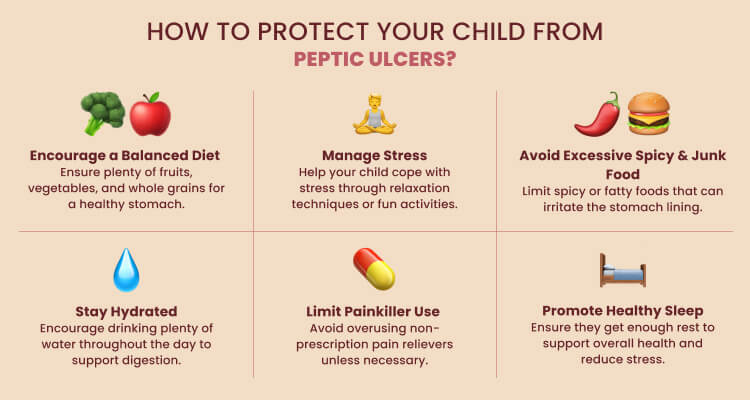
It’s easy to fall into the trap of thinking that acid peptic disease is an issue for older adults only. However, the truth is that this condition can affect people of all ages, including children and young adults.
Diet, lifestyle habits, and genetic factors influence your risk. In fact, H. pylori infections are commonly found in children, underscoring the importance of awareness for everyone. From a holistic perspective, maintaining a healthy gut involves more than just treating symptoms—it requires a balance of diet, lifestyle, and emotional well-being.
Listening to your body and addressing symptoms early—whether through dietary adjustments, herbal support, or mindfulness practices—can prevent long-term complications. If you experience persistent digestive issues, seeking professional guidance can help identify root causes and tailor a holistic approach for lasting wellness.
Myth 4: I’ll have to take medication for life if I have acid peptic ulcers.
Many people believe that once diagnosed with acid peptic ulcers, they will need to rely on medication permanently. However, this is not necessarily true. While medications such as proton pump inhibitors (PPIs) or H2 blockers may be prescribed for short-term relief and healing, long-term management can often be achieved through dietary and lifestyle changes.
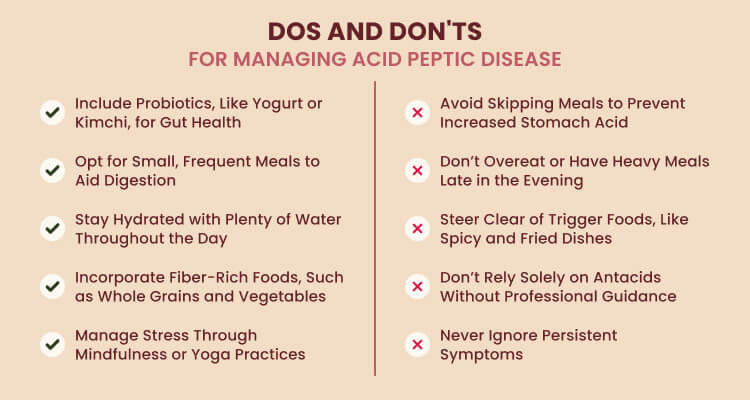
A gut-friendly diet plays a crucial role in ulcer healing and prevention. Take more fiber-rich foods, whole grains, seasonal fruits, vegetables, nuts, and seeds to promote digestive health and reduce inflammation. On the other hand, limit sugar, processed foods, fried items, alcohol, caffeine, and acidic foods like tomatoes and citrus that can prevent irritation of the stomach lining.
Additionally, managing stress, avoiding smoking, and adopting mindful eating habits can support long-term ulcer healing. In many cases, if the root cause—such as H. pylori infection—is treated, and dietary changes are maintained, the need for lifelong medication can be avoided.

Myth 5: Antacids alone can cure peptic ulcers.
You might say, “I just take antacids whenever I feel discomfort.” However, while antacids can provide temporary relief from ulcer symptoms by neutralizing stomach acid, they do not address the underlying causes of peptic ulcers.
Most ulcers are caused by either H. pylori infection or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin. Simply taking antacids does not eliminate H. pylori bacteria or heal the stomach lining from NSAID-induced damage. A proper treatment plan may include antibiotics (for H. pylori), proton pump inhibitors (PPIs), or H2 blockers, along with dietary and lifestyle changes.
Following a gut-friendly diet can support healing. Avoiding spicy foods, fatty and fried foods, alcohol, caffeine, citrus fruits, tomatoes, and chocolate can prevent irritation. Instead, focusing on a balanced diet rich in fiber, lean proteins, and gut-soothing foods can promote long-term digestive health.

Myth 6: I believe stomach peptic ulcers are not a serious health condition.
Some might underestimate their stomach issues, thinking, “It’s just a little discomfort; how serious can it be?” However, downplaying digestive issues can be risky. While mild cases may cause discomfort, persistent ulcers can result in internal bleeding, perforation (a hole in the stomach or intestine), and even life-threatening infections like peritonitis. Additionally, long-term ulcers increase the risk of stomach obstruction, making it difficult for food to pass through the digestive tract.
Ignoring symptoms such as persistent abdominal pain, nausea, vomiting (especially with blood), unexplained weight loss, or black, tarry stools can be dangerous. If you suspect you have a peptic ulcer, it’s essential to seek medical advice early. Prompt treatment can prevent complications and ensure long-term digestive health.
Myth 7: I don’t have any symptoms like heartburn, so I can’t have acid-peptic disease.
It’s easy to think that if you don’t have classic symptoms like heartburn, you’re in the clear. But acid-peptic disease (APD) isn’t always obvious. Some people go for months—or even years—without realizing they have it because the symptoms can be silent or unusual.
Instead of heartburn, you might feel bloating, nausea, fatigue, or even a loss of appetite. Some people only find out they have an ulcer when it starts bleeding, leading to anemia or black, tarry stools. Others don’t notice anything until they develop serious complications like a perforated ulcer (which is as painful as it sounds).
Just because you’re not feeling the burn doesn’t mean your stomach isn’t struggling. Pay attention to small signs, like frequent indigestion, unexplained discomfort, or changes in appetite. And even if you feel fine, taking care of your gut—by eating more fiber, cutting back on alcohol and fried foods, and managing stress—can go a long way in preventing problems before they start. If something feels off, don’t ignore it. Your stomach will thank you later!
Myth 8: I can reduce peptic ulcer symptoms by eating less.
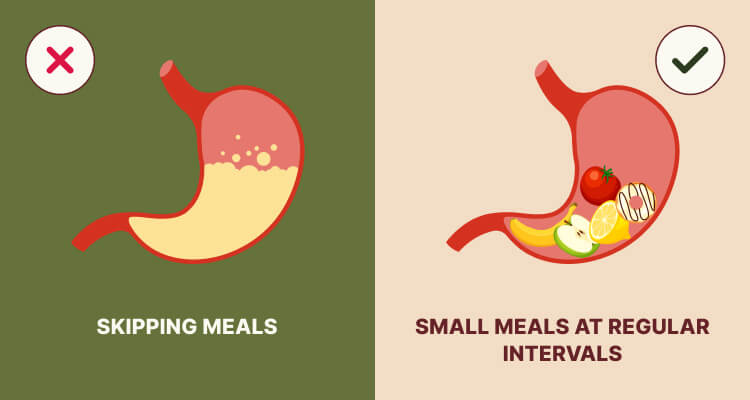
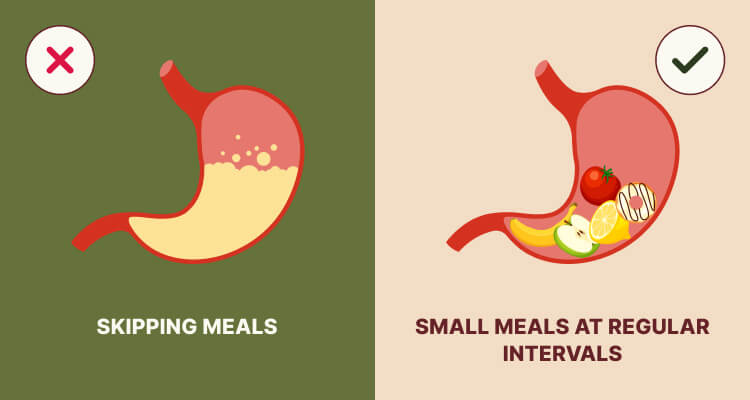
It might seem logical to eat less if you have a peptic ulcer—after all, less food means less acid, right? Not exactly. In reality, skipping meals or eating too little can make ulcer symptoms worse. When your stomach is empty for too long, acid levels can build up, irritating the ulcer and leading to more pain, bloating, and discomfort.
Instead of eating less, focus on eating the right foods in smaller, frequent meals. Foods rich in fiber, lean proteins, and probiotics—like oats, bananas, yogurt, and vegetables—can help soothe the stomach and support healing. On the other hand, skipping meals or going long periods without food can trigger more acid production, making symptoms worse.
If you have a peptic ulcer, it’s not just about how much you eat, but what and when you eat. Listening to your body and eating mindfully can help keep symptoms in check and promote healing.
Myth 9: I’ll always have chronic acid peptic ulcers.
Some may worry that being diagnosed means they’ll have to deal with ulcers for the rest of their lives. However, that’s not the case for everyone. The truth is, most ulcers can be healed with the right treatment and lifestyle changes.
In addition to medical treatments, Ayurveda, an ancient system of healing, offers a holistic approach to help manage and prevent ulcers. Ayurveda focuses on balancing the body’s energies, or doshas, to promote healing. For ulcers, this often means focusing on cooling foods and herbs that soothe the stomach, like aloe vera and licorice root. Ayurveda also suggests avoiding spicy, acidic foods and managing stress with practices like yoga and meditation.
Whether you prefer modern medicine or natural remedies, the key is that ulcers can heal with the right approach, and you don’t have to live with them forever.

Getting Real About Peptic Ulcers: A Holistic Perspective That Clears Up Myths
Now that we’ve debunked some common myths about acid peptic ulcers, it’s essential to explore a holistic approach to managing this condition. In Ayurveda, peptic ulcers are often referred to as Amlapitta. It is a traditional perspective that emphasizes the importance of individual symptoms and tailored treatments.
Ayurvedic practitioners begin by identifying the causes of Amlapitta, which can be categorized into four groups:
- Dietary Factors: Incompatible food combinations, excessive intake of Pitta-aggravating foods, and faulty eating habits (like untimely meals).
- Habit Factors: Poor lifestyle habits such as irregular sleep patterns and suppressing natural urges can disrupt the digestive balance.
- Psychogenic Factors: Emotional stress and negative psychological states can impact digestion, exacerbating symptoms.
- Miscellaneous Factors: External factors, including medication side effects, can also contribute to ulcers.
How Can You Embrace Holistic Healing for Peptic Ulcers?
When it comes to treating ulcers, Ayurveda takes a personalized approach, focusing on your unique body constitution and the specific manifestation of your condition. There are three main principles at play here:
-
Balancing Doshas
Here, the focus is on calming your Pitta dosha, which is often aggravated in cases of APD. It involves using herbs and drugs with cooling properties, like Ativisha and Patola, which help soothe irritation and promote healthy digestion.
In Ayurveda, maintaining balance in the body is crucial for good health. It often means reducing excess heat and acidity in the digestive system. Ayurvedic practitioners may recommend natural remedies and herbs known for their soothing properties. For example, licorice is recognized for its ability to coat and protect the stomach lining, while raisins or grapes can aid digestion and provide nourishment, making them beneficial for those experiencing ulcers.
-
Avoiding Aggravating Factors
A significant part of managing peptic ulcers involves avoiding foods that can worsen your condition. An Ayurvedic practitioner will help identify which foods might be irritating for you. Typically, it includes spicy dishes, caffeine, and alcohol, which can increase acidity and discomfort. Instead, you’ll be encouraged to focus on gentle, nourishing foods like fruits, vegetables, and whole grains that promote healing and comfort in your digestive system.
-
Lifestyle Changes
In addition to dietary adjustments, embracing holistic healing also means making positive lifestyle changes. Techniques such as yoga, meditation, and deep breathing can help reduce stress, which is essential since stress can exacerbate digestive issues. Regular physical activity that feels good for your body can further support overall health and digestion.
-
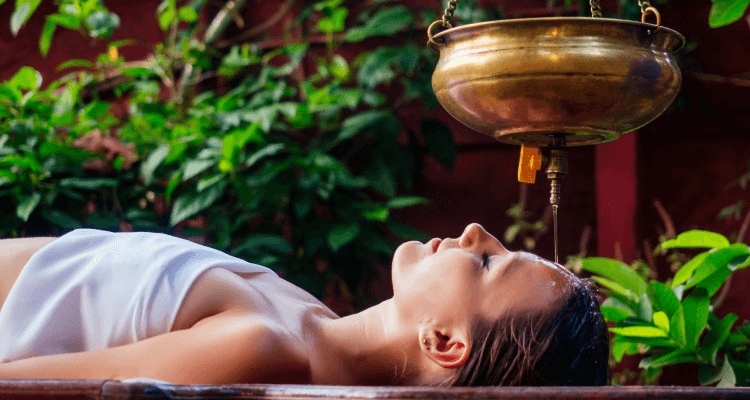
Panchakarma Therapies
Panchakarma is a powerful Ayurvedic detoxification process that is often utilized as a final step when other treatments have not achieved the desired results. It is a comprehensive approach used to remove accumulated toxins from the body. While it is an advanced therapy, it can provide profound healing benefits for individuals who have not found relief through other methods. By addressing the root causes of ailments, Panchakarma rejuvenates the body and promotes overall well-being, making it a valuable option for those seeking to enhance their health and vitality.
These detoxification therapies are tailored to your specific needs based on your type of APD:
- Therapeutic Emesis: Targets issues in the upper digestive tract.
- Purgation: Aids clearing excess toxins from the lower digestive tract.
- Medicated Enema: Effective for chronic cases, helping restore balance after assessing your digestive fire.
Are You Ready to Nurture Your Digestive Health?
Navigating the complexities of Acid Peptic Disease can feel daunting, but Ayurveda offers us a path that emphasizes understanding, balance, and holistic healing. By recognizing the root causes and making mindful choices, we can transform our approach to digestive health.
At LYBL, we are committed to integrating traditional wisdom with modern science, offering personalized care tailored to our needs. By embracing this holistic approach, we can live our best lives—healthier, happier, and more balanced.